Parkinson’s disease (PD) is often described as a movement disorder, but anyone living with it knows that its impact goes far beyond that. From subtle changes in voice to challenges with memory, mood, and expression, Parkinson’s can affect how we connect and communicate with the people we love most. For individuals with PD and their care partners, whether a spouse, family member, or close friend, communication is one of the most important tools you have to navigate this journey together.
The good news? Communication doesn’t have to be perfect, as long as you’re caring, respectful and open to learning.
Why communication can feel hard
Many people with PD experience changes that affect how they speak or engage in conversation. These might include a softer voice, trouble expressing emotion, slowed thinking, or fatigue during long discussions. On the care partner side, it can be difficult to know how to respond or when to bring up important topics. You might both feel like you’re walking on eggshells, or that you’re having the same conversation over and over.
These challenges can lead to misunderstandings, emotional distance, or frustration on both sides. But with small adjustments and a team mindset, communication can become a tool for connection rather than a source of tension.

How can we adopt a “team” mindset?
It’s easy to fall into the roles of “caregiver” and “patient,” where one person feels responsible for managing everything and the other feels like they’re being managed. Instead, try to see yourselves as partners. Use language that reflects shared responsibility and support, for example, “Let’s figure this out together,” or “What do you think would work best for both of us?”
This shift from “me vs. you” to “us vs. the problem” helps reduce blame and builds a sense of mutual respect and collaboration.
Different conversations, call for different approaches
There’s no one-size-fits-all formula for a good conversation. Depending on the topic, you might find yourselves having:

Recognizing the type of conversation can help you approach it with the right tone and expectations. And remember, what feels minor to one person may feel major to the other. Approach every topic with care and curiosity.
What are some tips for talking about the tough stuff?
Some topics, like changes in roles, emotional closeness, or long-term plans, are hard to bring up. Here are a few strategies that can help:
- Choose a quiet, private space, and unrushed moment
- Use “I” statements to share your experience (e.g., “I’ve been feeling a bit overwhelmed”)
- Avoid rushing to fix the problem, sometimes just listening is enough
- Emphasize teamwork: “Can we think this through together?”
- If things get tense, take a short break and return later.
These small adjustments can help create a safer space for meaningful conversation.
Everyday Strategies That Make a Big Difference
Simple communication strategies can improve understanding and reduce stress:
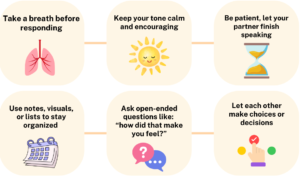
These tools aren’t just for big conversations, they’re useful every day.
Softer ways to say hard things
It’s easy to speak out of frustration, but a small shift in wording can make a big difference. Instead of saying, “You never help me,” try, “I’m feeling overwhelmed, can we talk about how to share the load?” Or instead of, “You’re not the same,” try, “I’ve noticed some changes. Can we talk about how we’re both feeling?” These more compassionate phrases open the door for honest, productive conversations.
Connection Beyond Conversation
Communication isn’t only about talking. Sometimes, the best connection comes through shared moments like a morning coffee, a short walk, listening to the birds, making dinner together, doing yoga, a puzzle, or watching a favorite movie.

These quiet routines create space to reconnect without needing to say much at all.
Creating rituals, like a weekly check-in or a “no-PD talk” evening, can help you stay grounded and emotionally close, even during difficult periods.
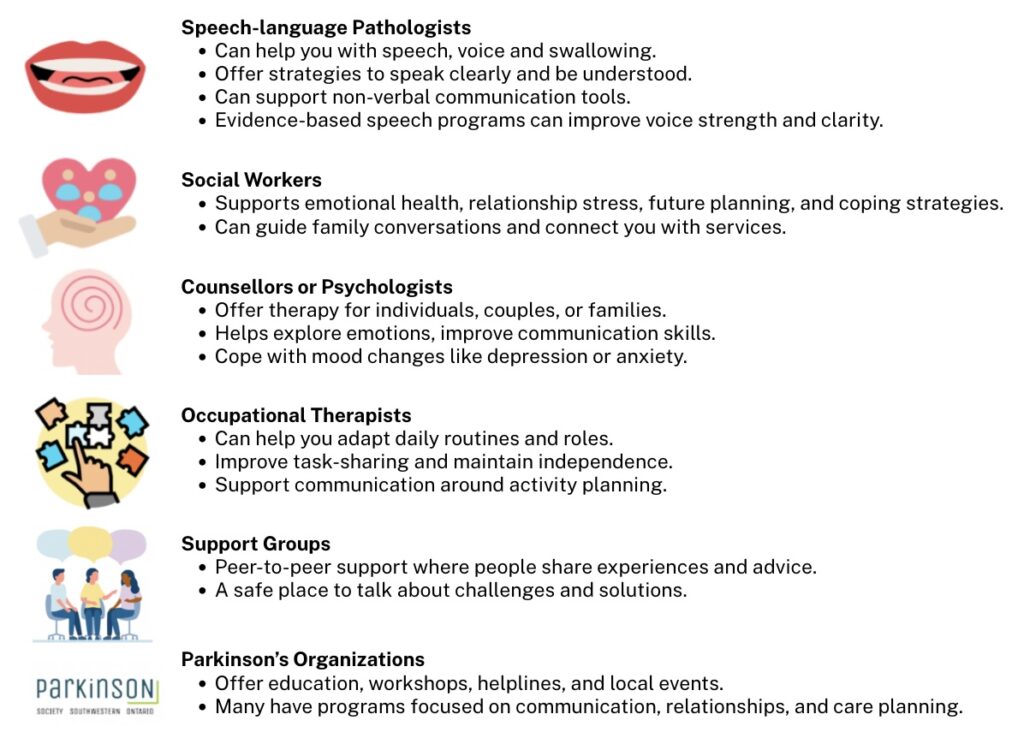
Who to Reach Out to for Help
If communication feels especially challenging, there are people who can help you. Your doctor, health team and/or the PSSO referral specialist can help connect you with the supports that you need.
Some conversations will be easier than others, and that’s okay. What matters most is your willingness to keep showing up for each other. Communication takes effort, but it’s also an act of care. You don’t need perfect words, just patience, openness, and a shared commitment to staying connected, no matter what comes your way.
This article was based on a research article published by Dr. Jeff Holmes, the author of this article, Olivia Crozier (a PhD student) and other researchers from the University of Western Ontario.

Olivia is a third-year PhD candidate at Western University completing a combined research (PhD) and Master of Science of Occupational Therapy program. Supervised by Dr. Jeff Holmes, her research focuses on improving health services and programs for people with Parkinson’s disease and their care partners in Southwestern Ontario.
